Avalon can help Centene realize up to 15% health plan savings on outpatient routine lab spend
By analyzing Centene's membership, we found potential savings of approximately $175 million per year.
Avalon’s Routine Test Management (RTM), streamlines the process of determining coverage criteria to eliminate unnecessary utilization of high-volume, low-cost laboratory tests while ensuring that providers and members are unaffected.
Submit the form to learn how Avalon and a health plan partnership resulted in $112M in annual savings.
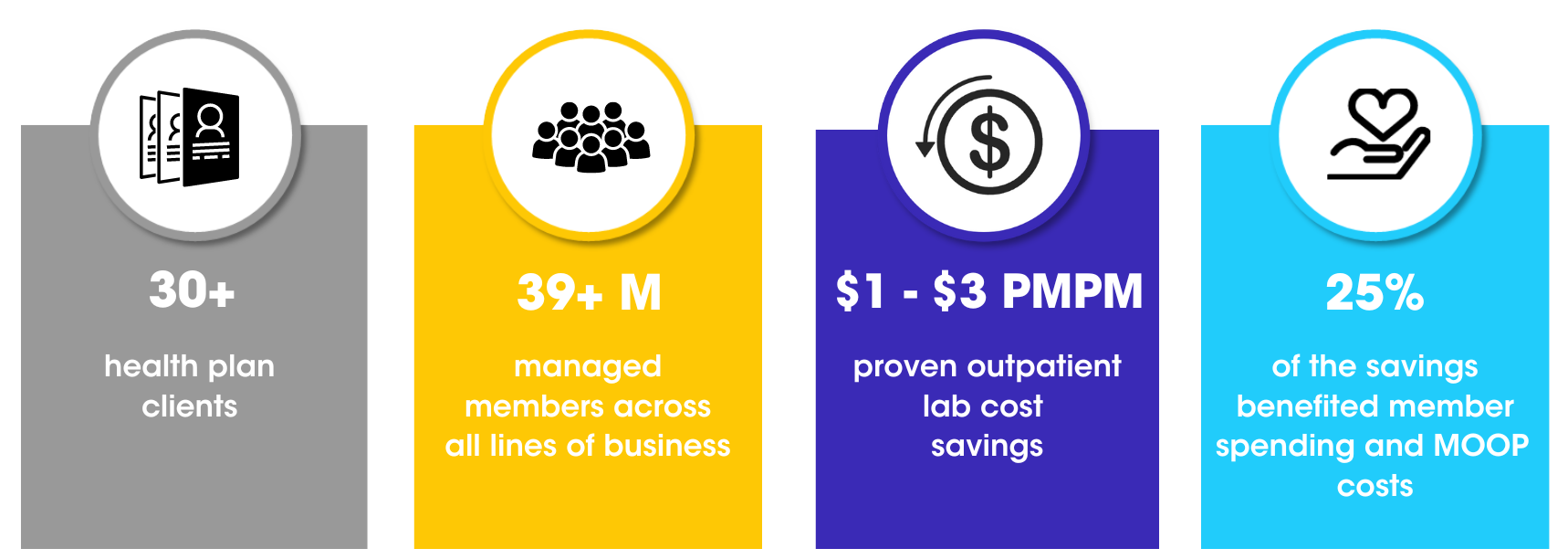
The Value Avalon Can Provide Centene

$1-$3 PMPM Savings
Estimated plan savings on outpatient lab spend
Decrease Appeals
Low provider reconsideration & member appeal rates
Lab Expertise
Lab policy expertise, proven evidence based-lab policies
& provider education

Automation
Automated real-time reimbursement policy enforcement
Despite their importance, ~ 30% of lab tests conducted in the U.S. are unnecessary, while another 30% of patients do not receive the testing they need.
Industry Challenge
• Increased administrative burden to manually monitor high-volume, low-cost claims such as routine lab testing
• Rendering lab overutilization behavior is consistent across payers and lines of business
• Site of service variation is significant, with hospital outpatient labs costing 575% more than independent labs
• Complexity in managing increased member and provider appeals
How are you managing the most utilized medical benefit: Lab Testing?
When it comes to meeting the needs of Centene and, importantly, your members, you need a partner who is committed to helping you realize significant savings for your organization and the members you serve. Avalon provides an innovative approach to ensure the right lab tests are provided at the right time for the right care and at the right cost.
Lab tests are an essential part of healthcare. As many as 70% of clinical decisions are guided by a test result, with data from the test informing care and improving patient outcomes. The number and sophistication of lab tests are on the rise, with approximately 14 billion clinical lab tests performed annually, which makes informed and consistent test management even more important.
Our unique automated solution can be customized to Centene's requirements, ensuring effortless compliance with routine lab policies
About Avalon

Download the 2024 Lab Trend Report Highlights Infographic to learn more about the important lab trends that affect health plans lab spend.
Blog Post
Discover the Hidden Benefits of Lab Benefit Management for Health Plans and Members
Physician Abrasion: An Understated Yet Crucial Concern for Payers
Blog Post
Why Testing Prices Vary Wildly Based on Location and What It Means for Your Health Plan
Transform Cancer Care with Advanced Oncology Drug Management